When couples face difficulties conceiving, the focus often tends to be on the female partner. However, male infertility is a significant factor that can contribute to difficulties in conception. Addressing infertility comprehensively requires evaluating both partners, as male fertility issues are quite common and can play a crucial role in the overall reproductive health of a couple. Here’s an in-depth look at why and how to consider evaluating your male partner for infertility.
Understanding Male Infertility
Male infertility is defined as the inability of a man to impregnate a partner after a year of regular, unprotected intercourse. It affects approximately 1 in 20 men, with varying degrees of severity. The causes of male infertility can be diverse and may include:
- Sperm Production Issues: Problems with the quantity or quality of sperm produced can hinder conception. Conditions like azoospermia (no sperm production) or oligospermia (low sperm count) are examples.
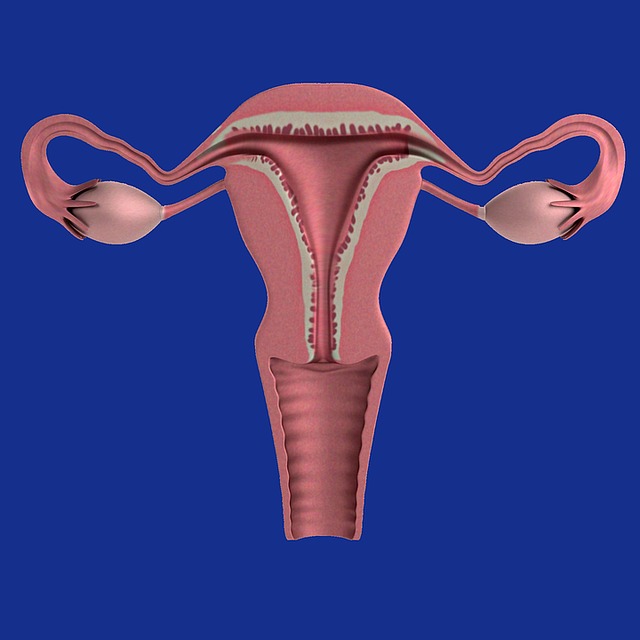
- Sperm Transport Problems: Blockages or abnormalities in the reproductive tract can prevent sperm from reaching the female reproductive system.
- Hormonal Imbalances: Disorders affecting hormones that regulate sperm production can lead to infertility.
- Genetic Factors: Genetic abnormalities, such as Klinefelter syndrome, can impact sperm production and quality.
- Lifestyle Factors: Factors such as smoking, excessive alcohol consumption, drug use, and poor diet can adversely affect sperm quality and fertility.
- Environmental and Occupational Hazards: Exposure to certain chemicals and toxins can impact sperm production and quality.
Why Evaluate the Male Partner?
- Comprehensive Diagnosis: Infertility is a complex issue, often involving multiple factors. While a female partner’s reproductive health is critical, neglecting the male partner’s role can result in an incomplete diagnosis. Approximately 40-50% of infertility cases are attributed to male factors alone or in conjunction with female factors.
- Avoiding Unnecessary Treatments: If the male partner’s fertility issues are not addressed, the female partner might undergo unnecessary treatments or procedures. Proper evaluation ensures that both partners receive appropriate and targeted interventions.
- Effective Treatment Planning: Understanding both partners’ fertility statuses helps in creating a well-rounded treatment plan. Treatments for male infertility might include medication, lifestyle changes, or assisted reproductive technologies like intrauterine insemination (IUI) or in vitro fertilization (IVF).
- Emotional and Psychological Support: Infertility can be stressful for both partners. Recognizing that male infertility is a shared concern can help in reducing emotional burden and promoting a supportive approach to treatment.
When to Consider Evaluation
- Prolonged Difficulty Conceiving: If a couple has been trying to conceive for over a year without success, it is advisable to evaluate both partners. The standard recommendation is to seek evaluation after six months of trying for women over 35, but this should be extended to both partners.
- History of Reproductive Health Issues: If the male partner has a history of conditions known to affect fertility (e.g., testicular injuries, surgeries, or chronic illnesses), an evaluation is warranted.
- Lifestyle and Environmental Concerns: Significant lifestyle or environmental factors affecting the male partner’s health should prompt an evaluation. These include high-stress jobs, exposure to hazardous substances, or substance abuse.
- Unexplained Infertility: In cases where the female partner has undergone evaluations and no clear issues have been identified, investigating male fertility becomes crucial to uncover any underlying problems.
Evaluation ProcessMedical History Review:
The evaluation typically begins with a thorough medical history, including lifestyle factors, previous medical conditions, and family history of genetic disorders.
- Physical Examination: A physical examination can help identify any anatomical abnormalities or signs of hormonal imbalances.
- Semen Analysis: This is a primary test for male infertility, assessing sperm count, motility (movement), morphology (shape), and overall quality.
- Hormonal Testing: Blood tests to measure hormone levels such as testosterone, follicle-stimulating hormone (FSH), and luteinizing hormone (LH) can help identify hormonal imbalances.
- Genetic Testing: If there are indications of genetic abnormalities, such as abnormal semen analysis results, further testing may be conducted to identify genetic causes.
- Imaging Studies: In some cases, ultrasound or other imaging techniques may be used to examine the reproductive organs for structural issues.
Read also: Male infertility myths and facts
Conclusion
Evaluating both partners for infertility is essential for a comprehensive understanding of reproductive health and effective treatment planning. Male infertility is a common issue that can significantly impact a couple’s ability to conceive, and addressing it can lead to better outcomes and reduce unnecessary stress. If you and your partner are facing challenges with conception, seeking a thorough evaluation for both partners can provide clarity and guide you toward appropriate and effective solutions.